While there are many options for replacement, dental implants are one of the most effective ways to replace a missing tooth to restore a smile. The biggest benefit of dental implants is that the implant will look no different than the other natural teeth and will support a patient’s oral health for years to come. Keep reading to learn about the different types of dental implants and dental implant materials to discover which type of implant is best for your needs.
When a tooth is lost due to injury or disease, a person can experience complications such as rapid bone loss, defective speech, or changes to chewing patterns that result in discomfort. Replacing a lost tooth with a dental implant can significantly improve the patient’s quality of life and health.
What are dental implants?
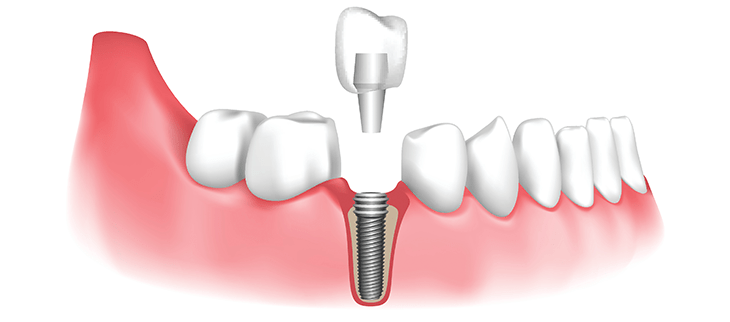
A dental implant is a structure that replaces a missing tooth. With precision and skill, the dentist inserts an implant into the jawbone, and it acts as an anchor for an artificial tooth, called a crown.
A device called an abutment connects the artificial tooth to the dental implant.
The crown is custom-made to fit the person’s mouth and match the color of their teeth. Crowns look, feel, and function like natural teeth.
Implants have several advantages
- are more natural and comfortable
- have a higher success rate
- improve chewing function
- lead to a lower risk of cavities developing in nearby teeth
- lead to better maintenance of bone at the site of the lost tooth
- cause decreased sensitivity in nearby teeth
- do not need to be taken out and cleaned every night
However, dental implants are not suitable for everyone. The implanting devices must bond with the jawbone, so a person’s bones must be healthy before they can undergo implant surgery.
What are the different types of dental implants?

There are two main types of dental implants and two main types of procedure, endosteal and subperiosteal, and single-stage and two-stage, respectively. All of the options are incredibly natural-looking but are used for different reasons. Your dentist will be able to guide you in making the right implant decision for your oral needs, but it is important to know the difference.
Endosteal
An endosteal implant is the more common of the two types of implants and what most dentists prefer to use. This type of implant is anchored into the jawbone to act as an actual tooth root and is shaped like a small screw. Dentists prefer to use this method because when a tooth is missing in the mouth structure it can cause bone loss and shift adjacent teeth. Endosteal implants anchored into the vacant tooth root helps preserve the structure of the face and jawbone.Subperiosteal
Subperiosteal implants look the same as endosteal implants but are completely submerged under the bone.
Oftentimes, dentists will suggest their patients to undergo a bone augmentation to rebuild and strengthen their jawbone so that they can receive an endosteal. If a patient does not want a bone augmentation however, they can achieve very similar results with a subperiosteal implant.
Single Stage
A single-stage dental implant requires only one surgical appointment. During the procedure, your dentist will place a longer implant into the jaw and gum so that the top of the implant is exposed. Once the area heals, the connector and crown parts of the implant will be attached right onto the exposed part of the implant.
The single-stage procedure is often used on patients with bone problems or those who have special needs. This is because the single-stage process is typically quicker once the initial surgery is done and the patient will have an easier adjustment to their new teeth.
Two-Stage
The two-stage dental implant procedure takes much longer than a single-stage because it requires a minimum of two surgeries with healing time in between. During the first part of this process, your dentist will surgically place the base of the dental implant into the jawbone and then stitch it up to heal. Once the mouth has healed after a few months, another minor surgery will expose the base of the implant to attach the connector piece and crown of the implant.
Although this type of process is more invasive and complex, it provides long term benefits. During the time between the first and second surgery, the base of the implant will fuse to the jawbone to create a base that is as strong as a real tooth root.
Dental implant materials
For many years, titanium implants were the only material used in implant dentistry but as technology continues to evolve, so do our options. The two main materials used for dental implants are titanium and zirconia. There is an extensive amount of research and testing that goes into developing new implant materials including the chemical and physical properties. These dental materials must be resistant to fracturing and corrosion while having the proper microstructure and composition.
Titanium dental implants
To this day, titanium dental implants are the most commonly used material. One of the main benefits of using titanium material implants is that it does not disturb the jawbone. When the titanium implant is placed, the bone is still able to grow next to the implant as it would a natural tooth which allows the implant to last longer.
Titanium implants are also the most cost-effective and versatile option. Most titanium implants today are not made out of pure titanium and are actually titanium alloys. This allows the implants to be stronger and safer for those that are allergic to titanium. Titanium is a biocompatible material which means it closely resembles the human body making implant fusion to the bone easier.
Zirconia dental implants
Unlike titanium that has been around seemingly forever, zirconia implants are the most recent material to come to the dental implant industry. Many patients have concerns with metal allergies and putting metal into their body which makes zirconia implants a great, metal-free, implant option. Zirconia is also used for making bridges and crowns and the material is very hard and strong. This material also fuses to the bone very similarly to how titanium does.
One of the most prominent downfalls to zirconia implants is that they simply have not been around as long as titanium implants have, so the material has not had the same level of testing. Zirconia dental implants, however, do have two large advantages over titanium implants:
- There is no dark metal color showing through the gums
- While zirconia can fracture more easily than titanium, they are less susceptible to corrosion
Procedures
Each person is likely to have a different experience of dental implant surgery. Factors that may influence this include:
- the number of teeth requiring replacement
- the location of the implants within the jaw
- the quality and quantity of bone at the implant site
- the person’s underlying oral and systemic health
Depending on these factors, additional procedures may be necessary. These can include:
Sinus augmentation
Placing an implant in the upper jawbone is usually difficult because of the location of the sinuses.The surgeon may need to perform a sinus augmentation — a procedure to lift the floor of the sinuses to allow more bone to develop so that the implantation can be successful.
Ridge modification
Some people have a jawbone abnormality that prevents enough bone for an implant from developing. In such cases, a surgeon may need to perform a ridge modification.
This involves lifting the gum to expose the area of deformed bone. The surgeon will then use a bone or bone substitute to repair and build up the area. This improves the quality of the jawbone in preparation for dental implant surgery.
Recommendations for Patients
Before choosing the best dental implants, talk to your dental provider about the potential benefits and risks, and whether you are a candidate for the procedure.
Things to consider:
- Your overall health is an important factor in determining whether you are a good candidate for dental implants, how long it will take to heal, and how long the implant may stay in place.
- Ask your dental provider what brand and model of dental implant system is being used and keep this information for your records.
- Smoking may affect the healing process and decrease the long-term success of the implant.
- The healing process for the implant body may take several months or longer, during which time you typically have a temporary abutment in place of the tooth.
After the dental implant procedure:
- Carefully follow the oral hygiene instructions given to you by your dental provider. Regularly cleaning the implant and surrounding teeth is very important for long-term success of the implant.
- Schedule regular visits with your dental provider.
- If your implant feels loose or painful, tell your dental provider right away.
Benefits of Dental Implant Systems:
- Restores the ability to chew
- Restores cosmetic appearance
- Helps keep the jawbone from shrinking due to bone loss
- Preserves the health of the surrounding bone and gums
- Helps keep adjacent (nearby) teeth stable
- Improves quality of life
Risks Associated with Dental Implant Systems:
- Damage to surrounding natural teeth during implant placement
- Injury to the surrounding tissues during surgery, such as sinus perforation
- Injury during surgery (for example, fracture of surrounding jawbone)
- Inadequate function, such as feeling like the teeth do not bite together normally
- A sensation that the tooth is loose or twisting in place resulting from an abutment screw loosening
- Implant body failure (looseness of the implant body)
- due to systemic infection, which may be more likely in patients with uncontrolled diabetes
- due to local infection in bone and gums supporting the implant body
- due to delayed healing, which may be more likely in patients who smoke
- Difficulty cleaning the gums around the implant, resulting in poor oral hygiene
- Untreated periodontal disease
- Post-surgical numbness due to nerve impingement or damage
- Always notify health care providers and imaging technicians that you have dental implants before any magnetic resonance imaging (MRI) or x-ray procedures. Dental implants can distort or interfere with these images. FDA is not aware of any adverse events reported for MRI or x-ray procedures with dental implants.
What to expect as a patient
The following should be done before the procedure:
• An elaborate dental examination
• Developing a plan for the surgery
• Disclosure of medical conditions and medications
• Discussing the mode of pain relief
• Scheduling the surgery
During the surgery, the anesthesia used by the dentist may make you feel groggy for some time. Incisions made in your gums to place the implant in the jaw may cause bruises, swelling, minor bleeding, and pain. The dentist may prescribe medication.
After the procedure, the gums are closed to cover the implant. You will be scheduled for a second phase of the procedure after a few months. After healing of the gums, an artificial tooth will be placed on the implant.
Pre care requirements
The following should be observed before dental implant procedures.
• Stop alcohol and tobacco use at least two weeks before the surgery because they can cause complications after surgery and inhibit the healing process.
• Disclose any medications you are taking to help your doctor take precautions to reduce the risk of complications.
• Practice proper oral hygiene to reduce bacteria that may cause infections in the gums after surgery.
• Plan your journey to and from the hospital because it may be unsafe for you to drive after the procedure.
• Prepare for the recovery period by getting items you may require during that period.
Post care suggestions
• Discomforts emanating from the procedure can be managed using over the counter painkillers.
• Ice can be placed on the area intermittently during the initial 24 hours to minimize swelling.
• Antibiotics prescribed to prevent infections must be taken to completion.
• Stick to soft foods to avoid disturbing the surgery area.
• Avoid hot drinks and spicy foods for a few days.
• Do not bite hard substances in the area of the implant until you have fully recovered.
• Be cautious when cleaning your teeth to avoid disrupting healing. Use Q-tip and appropriate cleaning solutions rather than a toothbrush.
• Stay away from strenuous activities for some time after the surgery.
• Avoid smoking for at least two weeks after surgery.
• A bite guard can be used to prevent trauma on the implant site.
• Visit your dentist regularly for checkups and follow up.
Ways Dental Implants are Evaluated for Safety
Dental implants systems are typically made of materials that follow international consensus standards of the International Organization for Standardization (ISO) or ASTM International. These standards have details of what makes a safe material. Most dental implant systems are made of titanium or zirconium oxide. Other materials such as gold alloys, cobalt-based alloys, titanium alloys, or ceramic materials are sometimes used. The safety profiles of these materials are well-known.
Dental implant systems are evaluated according to international consensus standards. Biocompatibility testing, to show that bodily contact with the device does not cause complications like irritation or allergic reaction, is part of the evaluation that helps ensure the materials in the dental implant system are safe and do not cause adverse effects when implanted in people.








